Healthcare-Associated Infections (HAIs), or formerly known as nosocomial infections, are infections acquired by patients receiving treatment for a medical condition or surgery and considered adverse events that often occur during treatment (World Health Organization, 2011). HAIs are also a significant cause of morbidity and mortality (Agency for Healthcare Research and Quality, 2019). The occurrence of HAIs is more common in the middle and low-income countries, 5.7% and 19.1%, respectively, or three times higher than in high-income countries (Khan et al., 2017). HAIs in Southeast Asia accounted for approx-imately 75% of the incidence (World Health Organization, 2011).
One of the most common causes of HAIs is Staphylococcus aureus, a gram-positive bacteria that often causes various infections; MRSA is one (Bröker et al., 2016). World Health Organization (2011) reported that 5-10% of hospitals' infections are caused by Staphylococcus aureus, and the incidence is increasing every year. This increase has occurred in almost all regions of the world. Asia is the region with the highest incidence of infection across the globe. Indonesia is one of the countries with an increased incidence of infection with Staphylococcus aureus in Southeast Asia, approximately 28% (Chen & Huang, 2014).
The high incidence of this infection can be a mode of transmission, from patients to patients, patients to health workers, patients to medical equipment, health workers to visitors, and from health workers to other health workers and the environment (Khan et al., 2017; Price et al., 2017). Hand contact is the main transmission in its spreading mode (Levinson, 2010; Nazliansyah et al., 2016). Health care workers' hands play an important role in the transmission of HAIs, including nurses.
Cell phone is considered a convenient transmission medium for HAIs (Kanayama et al., 2017; Pillet et al., 2016), as it is rarely cleaned and frequently touched during or after examining patients without washing (Pal et al., 2015). Therefore, hand hygiene is recommended to be the primary measure necessary to reduce HAIs. Hand hygiene is also a key indicator in the infection prevention and control assessment for medical personnel (World Health Organization, 2018), especially for nurses who most often meet patients and take action on patients 24 hours of admission to a hospital. Given the explanation above, the purpose of this study was to determine the relationship between nurses' hand hygiene behavior with the colonization of Staphylococcus aureus on their cell phones in the intensive care unit.
Methods
Study Design
This study employed an observational design with a cross-sectional approach from December 2019 to January 2020.
Sample
The study population included nurses who worked at the intensive care unit of UGM Academic Hospital, Yogyakarta, Indonesia. The sample size was determined by total sampling. The inclusion criteria were a nurse who had a cell phone and always brought the cell phone to the intensive care unit. The exclusion criteria were a nurse who took extended leave, maternity leave or attended training or activities outside the hospital during the study. Total respondents were 38 nurses, but one respondent dropped out because of an injury in his right hand, so he could not perform proper hand hygiene.
Instrument
Nurses' hand hygiene behaviors were measured using the checklist sheets in the form of compliance behavior observations of hand hygiene following 'My five moments' approach adopted from Pittet et al. (2009), with the measurement results in the form of a percentage comparison between actions and opportunities. The five moments observed were 1) before touching a patient, 2) before clean/ aseptic procedure, 3) after body fluid exposure risk, 4) after touching a patient, and 5) after touching patient surroundings.
Colonization of Staphylococcus aureus was observed by implanting cell phone surface swabs on Nutrient Agar and Staphylococcus Agar media. After incubation at 37oC for 18-24 hours, the number of colonies that grew was counted by the total plate count method. Identification of Staphylococcus aureus was conducted according to the Standard Operating Procedure in the Microbiology Laboratory of the Faculty of Medicine, Public Health and Nursing (FKKMK UGM) (Granato et al., 2019).
Data Collection
Observations were made by the researcher and assisted by a research assistant, namely a master nursing student who has gained knowledge and practice related to procedures in bacterial identification. An interobserver test was done using the Intraclass Correlation Coefficient (ICC) with a test result of 0.988, which indicated the acceptable reliability of the two observers. Observations were made on nurses who were implementing nursing care during their shift. In making observations, the researcher did not tell the respondent who was observed in one shift to avoid bias. Each respondent was observed three times with a random observation time (a full hour for each observation).
Data Analysis
Univariate analysis was conducted to determine the characteristics of the respondents using the average distribution and frequency, including name, age, gender, last education, length of service, occupation, frequency of cleaning cell phones, cleaning materials, and length of time having a cell phone. Bivariate analysis was conducted to determine the relationship between hand hygiene beha-vior and bacterial colonization on nurses' cell phones. As data were not normally distributed (p < 0.05), the Spearman rank test was used to examine the relationship between hand hygiene behavior and the amount of colonization of bacteria. To identify the relationship between hand hygiene behavior and the presence of bacterial colonization, the Mann Whitney test was used. Statistical analysis was performed using SPSS version 21 software (IBM Corp., Chicago).
Ethical Consideration
This research has received ethical approval from the Medical and Health Research Ethics Committee of FKKMK UGM on 25 October 2019 with the number KE/FK/1267/EC/2019. After the researcher clearly explained the study's objectives, the respondents voluntarily signed the informed consent form to participate in the study. The respondents had the right to refuse to participate without penalty. We ensured that participants were not affected by any consequences in their work.
Results
Characteristics of Respondents
The majority of respondents were women (78.4%), and their average age was 29.6 years old, with the education level of registered nurses (64.9%) and the average length of work of 4 years. All of the respondents indicated they had never cleaned their mobile phones with agents such as alcohol (97.3%). Most respondents had their cell phones for over 12 months (81.1%) (Table 1).
| Characteristics | Average (Year) | f | % | |
|---|---|---|---|---|
| Age | 29.6 | |||
| Gender | Men | 8 | 21.6 | |
| Women | 29 | 78.4 | ||
| Education | Associate Degree | 13 | 35.1 | |
| B.N. + RN | 24 | 64.9 | ||
| Length of work | 4.0 | |||
| Never cleaned cell phones | Yes | 37 | 100.0 | |
| Material | Alcohol | 36 | 97.3 | |
| Non-alcohol | 1 | 2.7 | ||
| Length of having a cell phone | 0-3 months | 3 | 8.1 | |
| 4-6 months | 2 | 5.4 | ||
| 7-12 months | 2 | 5.4 | ||
| >12 months | 30 | 81.1 | ||
Hand Hygiene and Bacterial Colonization
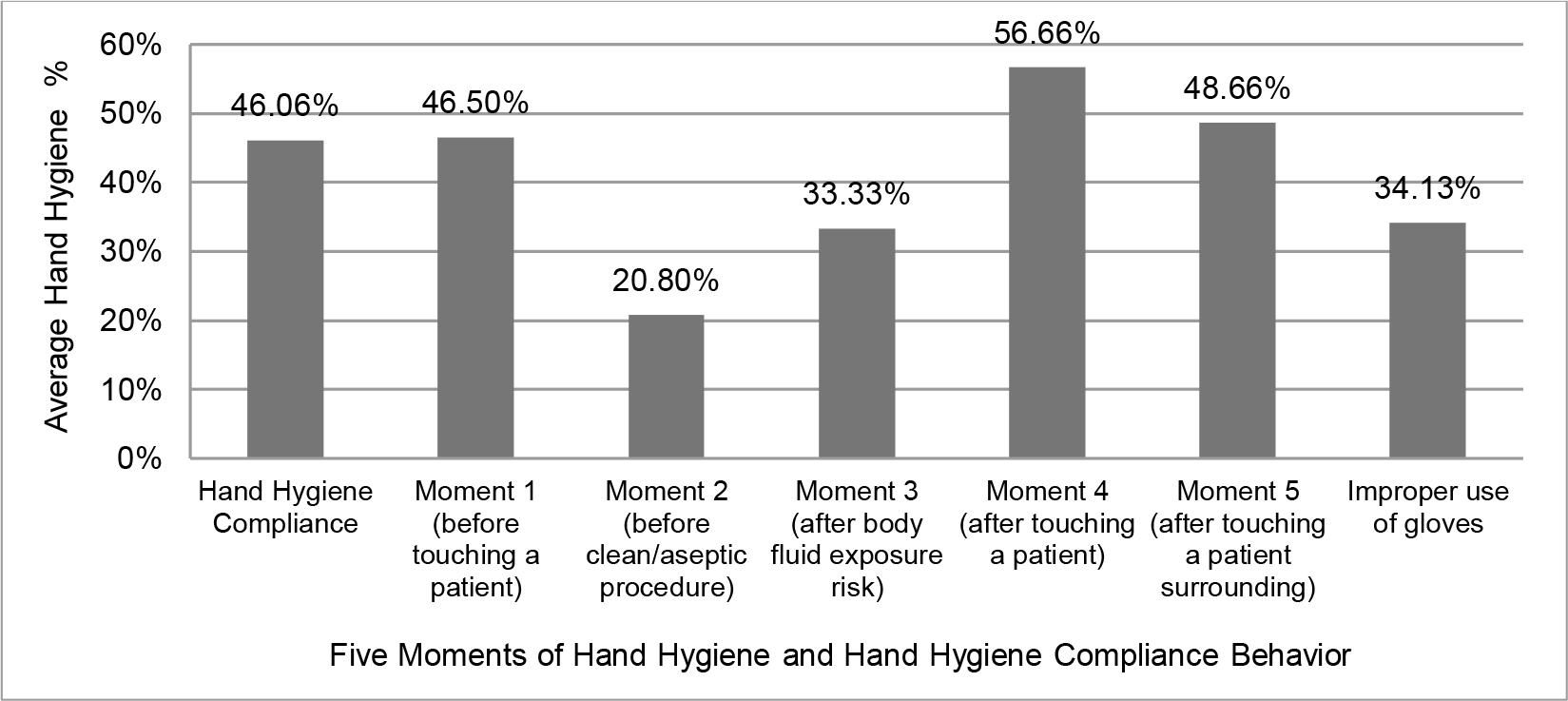
The highest average of nurses' hand hygiene behavior occurred at the moment 4 (after contact with the patient), 56.66%; while the lowest average occurred at the moment 2 (before action aseptic), 20% to 80%. The average of overall moments of hand hygiene was 46.06%. In this study, the use of gloves was also observed when performing hand hygiene. The result of observation showed 34.13% did not use gloves properly (Figure 1).
Gram-positive bacteria colonization was found on 35 respondents' cell phones (94.6%), and 24 (64.9%) of them contained Staphylococcus spp. Among all respondents, seven cell phones (18.92%) had Staphylo-coccus aureus colonization (Table 2).
| Average (CFU/ml) | Max (CFU/ml) | Min (CFU/ml) | f | % | ||
|---|---|---|---|---|---|---|
| Bacterial colonization | Gram-positive | |||||
| Positive | 35 | 94.6 | ||||
| Negative | 2 | 5.4 | ||||
| Amount | 507.84 | 15.000 | 0 | |||
| Gram-negative | ||||||
| Positive | 21 | 56.8 | ||||
| Negative | 16 | 43.2 | ||||
| Amount | 1927.57 | 70.000 | 0 | |||
| Staphylococcus spp. | ||||||
| Positive | 24 | 64.9 | ||||
| Negative | 13 | 35.1 | ||||
| Amount | 31.35 | 250 | 0 | |||
| Staphylococcus aureus | ||||||
| Positive | 7 | 18.92 | ||||
| Negative | 30 | 81.08 | ||||
| Amount | 5.41 | 100 | 0 |
The Relationship Between Hand Hygiene Behavior and Bacterial Colonization
Table 3 shows statistically no significant correlation between the nurses' hand hygiene behavior with either the number of bacterial colonization and the presence of bacteria Staphylococcus spp. and Staphylococcus aureus (p>0.05).
| Hand hygiene | p | |
|---|---|---|
| Bacterial colonization | Presence and absence of bacteria | |
| Staphylococcus spp. | 0.353 | |
| Staphylococcus aureus | 0.450 | |
| Number of bacteria | ||
| Staphylococcus spp. | 0.221 | |
| Staphylococcus aureus | 0.473 |
Discussion
Figure 1 shows that the average compliance behavior of respondents with hand hygiene was 46.06%, which is considered low. This is in line with Stahmeyer et al. (2017) reported an average hand hygiene adherence of 42.6%, and Selim and Abaza (2015) reported adherence ranging from 37-42%. These reports are of great concern because hand hygiene is the main measure for reducing HAIs and is a critical indicator for assessing infection prevention and control (World Health Organization, 2018). Sickbert-Bennett et al. (2016) reported that a 10% increase in hand hygiene adherence was associated with a 6% decrease in HAIs.
In this study, it was found that 34.13% of nurses did not use gloves according to the indication. The improper use of gloves may affect low adherence to hand hygiene. Health care workers or nurses often remove their gloves after a single contact. Still, the gloves will only be changed when all courses of action are completed or when they are very dirty and need to be replaced (Kuzu et al., 2005), or at a change of action at different moments of patient interaction (Picheansathian & Chotibang, 2015). This is not in accordance with the recommendations established by the WHO guidelines (World Health Organization, 2009). Hand hygiene behavior affected by the improper use of gloves was reported by Moghnieh et al. (2017). The caregivers did not feel they needed to wash their hands before using gloves because they thought gloves already protect them.
Another aspect that indicates that the use of gloves was not appropriate is at the moment 2 (before aseptic action). The average percentage shows a low number (18.3%), in line with Picheansathian and Chotibang (2015). It is well known that wearing gloves does not prevent cross-infection. Therefore, strengthening education on the appropriate use of gloves indication should always be emphasized.
The length of time doing hand hygiene also affects behavior. According to Stahmeyer et al. (2017), the time spent on hand hygiene is 8.3 minutes in the intensive care unit. If nurses fully comply with the recommendation, then 58.2 minutes will be spent on hand hygiene for each patient during the shift.
The results of the surface swab of the cell phones showed that there were gram-positive bacteria (94.6%) and gram-negative bacteria (56.8%) on the nurses' cell phones. Colonization of Staphylococcus spp. was found on the cell phones of 24 respondents (64.9%) with an average number of bacteria, namely 31.35 CFU/m. A total of seven respondents (18.92%) had colonization of Staphylococcus aureus on their cell phones. These results are consistent with other studies showing that cell phone use in hospitals poses a risk of transmission of various bacteria, including pathogenic agents resistant to some drugs, such as Methicillin-Resistant Staphylococcus aureus (MRSA) (Curtis et al., 2018; Selim & Abaza, 2015). Cell phones can function as reservoirs for infection in health care settings (Kanayama et al., 2017; Smibert et al., 2018), with very high levels of contamination (Pal et al., 2015). The growth rate of pathogens or bacterial contamination is 40-100% on cell phones' surface, and the majority of these bacteria are potentially nosocomial pathogens that cause HAIs (Curtis et al., 2018). Staphylococcus aureus is drought tolerant and can survive and reproduce rapidly in warm environments such as cell phones (Trivedi et al., 2011).
The bivariate analysis revealed no relationship between hand hygiene behavior and Staphylococcus aureus colonization on nurses' cell phones. Poor hand hygiene will affect bacterial colonization growth on cell phones that occurs due to contact with hands. However, it was seen that the good bacteria were present, or there was no growth of bacterial colonization on cell phones, which is equally low with the value of hand hygiene behavior of nurses (46.06%), especially at the moment 2 (20.80%). The compliance value of hand hygiene that must be met is that it must exceed 80% (Ministry of Health, 2018) to influence the number of bacterial colonization. Still, it has not impacted the presence of bacterial colonization, seeing that the value of bacterial colonization is low.
Other factors can also affect the colonization of bacteria on cell phones, such as the possibility of contamination on cell phones obtained not directly from the patient or nurses' hands but obtained from the care environment where the cell phone is placed. The environment near or far from the patient can be a place for bacterial contamination (Wille et al., 2018). As for findings in the air, they are considered not a priority because these findings are less than direct contact with the environment or with patients and other health workers (Kozajda et al., 2019).
In our study, there was no relationship between hand hygiene behavior and colonization. After doing five moments of hand hygiene, certainly, nurses did not directly hold their cell phones. Still, they did other activities in the care area, either to write on patient medical records or to fill in data on a computer. However, when nurses wanted to use their cell phones, they did not wash their hands. Besides, the hand hygiene moments 4 and 5 (after touching a patient and after touching the patient's environment) showed that the average values of compliance behavior were only 56.66% and 48.66%. The habit of the respondents, who often hold their cell phones before the swab, also affects the number of bacterial colonies. The more frequent use of cell phones will increase the number of bacterial colonization (Hagel et al., 2019).
Another analysis that might result in no relationship between hand hygiene behavior and coloni-zation is related to hand hygiene measures. Besides being done at the right time, hand hygiene measures must also be done with the right steps. Doing hand hygiene with the proper techniques and materials will make hands free of potentially harmful contaminants and lower the risk of contaminating objects or other people (World Health Organization, 2009). Savolainen-Kopra et al. (2012) reported that washing hands with the correct techniques and materials would reduce the risk of contamination by 6.7%. Also, hands that are not dried or are not completely dry when finished washing their hands will increase the amount of bacterial contamination. Transmission of bacteria is more likely to occur from wet hands than dry hands (Huang et al., 2012). Generally, the number of bacteria on the palms is very large, namely 3.9x104 – 4.6x106 CFU/cm2 (Siegel et al., 2007), so it is possible to transfer to objects are touched by the hands. After washing hands, some bacteria on the palms remain (Pittet et al., 2009). Widodo et al. (2017) reported remain-ing around 55.2 CFU ml of bacteria after washing hands.
Hand hygiene measures are more effective if the hands' skin is free from wounds and has natural nails cut short so that no bacteria will remain between the nails, which will reduce transmission (Pittet et al., 2009). The fingers and hands are the parts that most frequently touch the cell phone when in use, so it is essential to perform hand hygiene to prevent transmission of the bacteria. Staphylococcus spp. or Staphylococcus aureus is normal in humans, especially in the nasal and skin areas (Taylor & Unakal, 2018). One of the factors that can cause the spread of pathogens is hand contact, so hand hygiene is crucial. Therefore, it is advisable to keep washing hands even though they are not in contact with the phone or contact the patient (Lin et al., 2017).
Besides, various other factors, such as the use of cover for mobile phones, can affect the colonization of bacteria on cell phones. The use of plastic as a wrapper for cell phones can reduce bacteria's growth by as much as 4.2 times (Manning et al., 2013). The use of cell phones together with colleagues can also affect contamination from bacteria, and it would be better if cell phones were not carried when conducting actions on patients (Bhoonderowa et al., 2014).
Based on the results of this study, hospital management can improve nurses' understanding related to infection control, namely by socializing about the use of gloves as indicated, hand hygiene, and limited use of cell phones to prevent cross-transmission. This research can be used as a basis for carrying out nursing practice and a reason for routine hand washing before and after using cell phones. The findings of this study also increase understanding about indications of glove use and regular cleaning of cell phones with a cleaning period.
The limitation of this study is that there was no examination of bacteria before the observation was carried out. So, it could not show whether there was a decrease or increase in bacterial colonization on cell phones due to hand hygiene. The colonization data were also taken immediately after three random observations, so the relationship of hand hygiene behavior might not be described accurately.
Conclusion
Nurses' hand hygiene behaviors at the intensive care unit were still low and could contribute to the colonization of Staphylococcus aureus on their cell phones. However, the results showed no relationship between the hand hygiene behavior and the colonization of Staphylococcus aureus on the cell phones of nurses. Further research is recommended to identify colonization before and after regular observations to determine whether there is any increase or decrease in colonization. Similar studies are also advised to conduct with larger sample size.